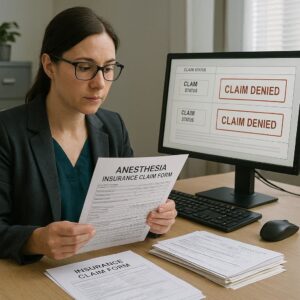
Navigating the world of medical insurance can feel like learning a foreign language, especially when a claim is unexpectedly denied. For patients and healthcare providers alike, an anesthesia insurance claim denial can be a source of significant stress, confusion, and financial burden. You’ve received the bill, seen the startling total, and then the denial letter arrives, often filled with codes and jargon that seem designed to obscure rather than clarify.
Why does this happen so frequently with anesthesia services? The reasons are often rooted in the unique nature of anesthesiology—it’s a specialized, procedure-based service that insurance companies sometimes view through a lens of complex rules and pre-authorization requirements. A denial is not necessarily the final word. In many cases, it’s the starting point of a process you can successfully navigate.
This guide is your essential resource. We will walk you through the entire landscape of anesthesia claim denials, from understanding why they happen to executing a strong appeal. Our goal is to empower you with knowledge, turning a frustrating setback into a manageable challenge.
Anesthesia Insurance Claim Denials
Understanding the “Why”: Common Reasons for Anesthesia Claim Denials
Before you can effectively fight a denial, you need to understand the battlefield. Insurance companies deny claims based on specific, albeit sometimes frustrating, criteria. Here are the most common culprits behind an anesthesia claim denial.
Lack of Medical Necessity
This is perhaps the most frequent reason cited. The insurance company asserts that the anesthesia services were not medically necessary for the procedure performed. This can happen if:
-
The payer believes the procedure could have been done under local anesthesia or conscious sedation.
-
The patient’s documented health status (ASA Physical Status classification) doesn’t align with the level of anesthesia billed.
-
The procedure itself is deemed elective or not covered, and by extension, the anesthesia for it is also denied.
Coding Errors and Mismatches
Anesthesia billing uses specific Current Procedural Terminology (CPT) codes and modifiers. A simple error can trigger an automatic denial.
-
Incorrect CPT Code: Using a general surgery code instead of a specific anesthesia code.
-
Missing or Wrong Modifiers: Anesthesia modifiers like AA (anesthesia performed personally by anesthesiologist), QK (medical direction of two, three, or four concurrent anesthesia procedures), or physical status modifiers (P1-P6) are crucial.
-
Mismatched Diagnoses: The diagnosis code (ICD-10) on the claim must justify the need for anesthesia for that specific surgical procedure. A mismatch here is a red flag for payers.
Failure to Obtain Pre-authorization or Pre-certification
Many insurance plans require prior approval for surgical procedures. If the pre-authorization was not obtained, was filed incorrectly, or only covered the surgeon’s fee and not the anesthesia service, the claim will be denied. This is often a breakdown in communication between the surgical office, the patient, and the anesthesia provider.
Out-of-Network Providers
This is a huge source of surprise bills. Even if your hospital and surgeon are in-network, the anesthesiologist or CRNA (Certified Registered Nurse Anesthetist) working that day may not be. Many patients are unaware they receive care from out-of-network providers in an in-network facility, leading to a denial of insurance claim or balanced billing for the difference.
Missing or Inadequate Documentation
The anesthesiologist’s record must thoroughly document the patient’s condition, the anesthesia plan, the duration of care, and any complications. If the documentation is sparse or doesn’t support the time units or complexity billed, the insurer will deny the claim requesting more information.
Benefit Plan Exclusions
Some plans have specific exclusions for certain types of anesthesia or for procedures considered experimental or cosmetic. It’s the patient’s responsibility to know their plan’s coverage, though this information is often buried in dense policy documents.
Comparative Table: Common Denial Reasons & Immediate Actions
| Denial Reason | What It Typically Means | Your First Step |
|---|---|---|
| Medical Necessity | Insurer doesn’t agree anesthesia was needed. | Request a detailed copy of the anesthesiologist’s notes. |
| Coding Error | A typo or incorrect modifier was used on the claim. | Contact the anesthesia billing office to verify codes. |
| Pre-authorization | Required permission was not secured before surgery. | Determine whose responsibility it was (surgeon’s office usually). |
| Out-of-Network | The anesthesiologist isn’t contracted with your plan. | Check your Explanation of Benefits (EOB) and state balance billing laws. |
| Documentation | The insurer needs more info from the medical record. | Work with the provider to ensure records are submitted promptly. |
Important Note: “A denial is not a rejection. It is a request for more information or a clarification of the services provided. The most powerful tool in reversing a denial is clear, complete, and compliant documentation.” – Common sentiment among medical billing advocates.
Your Step-by-Step Action Plan: Responding to a Denial
When you receive that denial notice, don’t panic and don’t ignore it. Follow this systematic action plan.
Step 1: Decode the Denial Notice
Your first document is the Explanation of Benefits (EOB) or denial letter. Look for:
-
Claim Number: Your reference number for all communication.
-
Denial Reason Code: A code like CO-50 (service not covered) or PR-1 (lack of pre-authorization).
-
Payer’s Contact Info: For the appeals department.
-
Appeal Deadline: This is critical. Missing this date usually forfeits your right to appeal.
Step 2: Gather Your Documents
Create a file with:
-
The denial letter/EOB.
-
The original itemized bill from the anesthesia provider.
-
Any pre-authorization documents you have.
-
Your insurance policy details (summary of benefits).
-
A copy of the surgical consent form.
Step 3: Initiate Contact
For Patients: Call your insurance company first. Ask for a clear, plain-language explanation of the denial. Then, call the anesthesia provider’s billing office. Often, they will handle the appeal for you, as they want to get paid.
For Providers: Conduct an internal audit. Review the chart, verify codes and documentation, and identify the likely error before contacting the payer.
Step 4: File a Formal Appeal
The appeal is your formal request for reconsideration. It must be in writing and include:
-
Patient and policy information.
-
Claim number and date of service.
-
A clear statement: “I am appealing the denial of claim [number] for anesthesia services on [date].”
-
A concise argument addressing the specific denial reason. Use facts from the medical record.
-
Copies of all supporting documents (highlighting relevant sections).
-
A request for a full and fair review.
Send the appeal via certified mail with a return receipt before the deadline. Keep copies of everything.
Step 5: Escalate if Necessary
If your first appeal is denied, you have further options:
-
Internal Second Appeal: Request a review by a higher-level medical director at the insurance company.
-
External Review: By law, you have the right to request an independent, third-party review if the internal appeals are exhausted. Your state’s insurance department can guide you here.
-
State Insurance Department Complaint: Filing a complaint with your state’s regulator can prompt action from the insurer.
-
Legal Counsel: For very large sums, consulting with a patient advocate or attorney specializing in insurance law may be warranted.
The Provider’s Perspective: Preventing Denials at the Source
The best anesthesia claim denial is the one that never happens. For anesthesia practices, a proactive approach is key to financial health and patient satisfaction.
Invest in Expert Billing and Coding
Ensure your billing staff is specially trained in anesthesia coding. Regular audits and continuing education are non-negotiable. Consider using anesthesia-specific billing software that checks for common errors.
Prioritize Impeccable Documentation
The medical record is your star witness in any appeal. Documentation must be:
-
Timely: Completed during or immediately after the procedure.
-
Accurate: Correct patient, procedure, times, drugs, and doses.
-
Complete: Includes pre-anesthesia assessment, intraoperative monitoring records, and post-anesthesia notes.
-
Compliant: Meets all standards set by the American Society of Anesthesiologists and payer guidelines.
Verify Benefits and Network Status Proactively
For scheduled procedures, a dedicated staff member should verify the patient’s anesthesia benefits and the practice’s network status with the payer before the day of surgery. If you are out-of-network, transparent communication with the patient, including potential cost estimates, is both ethical and legally required in many states.
Master the Pre-authorization Process
Develop a reliable system to confirm that pre-authorization for anesthesia is secured, not just for the surgery. Track authorizations and link them directly to the patient’s file.
Helpful List: Anesthesia Practice Denial-Prevention Checklist
-
Conduct monthly coding audits.
-
Provide ongoing documentation training for clinicians.
-
Implement a pre-surgery insurance verification protocol.
-
Assign a staff member to track and manage denials/appeals.
-
Foster clear communication channels with surgical facilities and surgeon offices.
-
Stay updated on changes to payer policies and state laws.
The Legal and Regulatory Landscape: Know Your Rights
Patients are not powerless. Recent laws provide new protections.
-
The No Surprises Act (NSA): Effective January 2022, this federal law protects patients from surprise bills for out-of-network emergency services and for out-of-network providers at in-network facilities (like anesthesiologists) without their consent. It establishes an independent dispute resolution (IDR) process for providers and insurers to settle payment disagreements, removing the patient from the middle.
-
State Balance Billing Laws: Many states have their own laws limiting or prohibiting out-of-network providers from “balance billing” patients for the difference between their charge and the insurer’s allowed amount.
Important Note: While the No Surprises Act is a powerful tool, it has specific rules and exceptions. It does not apply to all types of insurance plans (like grandfathered plans). Always check its applicability to your situation.
Conclusion
An anesthesia insurance claim denial can feel like a daunting roadblock, but it is most often a detour, not a dead end. Success hinges on understanding the precise reason for the denial, responding promptly and thoroughly with a well-documented appeal, and leveraging the protections offered by modern laws like the No Surprises Act. For providers, prevention through expert coding, flawless documentation, and transparent patient communication is the cornerstone of financial and operational stability. By approaching the process with knowledge and persistence, both patients and practitioners can navigate this complex aspect of healthcare with greater confidence and success.
Frequently Asked Questions (FAQ)
Q: I was asleep for my surgery. How could the anesthesia be “not medically necessary”?
A: From an insurance perspective, “medical necessity” means the service is appropriate and essential for the diagnosis and treatment of the condition. They may argue that a less intensive form of anesthesia (like a nerve block or sedation) was sufficient. The appeal must use the patient’s medical history and the surgeon’s notes to prove why general anesthesia was the only safe and appropriate option.
Q: The anesthesiologist was out-of-network at my in-network hospital. Am I responsible for the full bill?
A: In most cases, no. Thanks to the federal No Surprises Act, you are generally only responsible for your in-network cost-sharing amounts (copay, coinsurance, deductible) in this scenario. You cannot be balance billed for the remainder. The provider and insurer must work out the payment.
Q: How long does the appeals process typically take?
A: An internal appeal with an insurance company can take 30 to 60 days for a decision. If you escalate to an external review, it may take an additional 30-45 days. It’s crucial to meet all deadlines to avoid unnecessary delays.
Q: Should I stop the anesthesiologist on the day of surgery to ask about network status?
A: This is a difficult but important question. Ideally, this information should be provided to you well in advance by your surgeon’s office or the hospital. If you are unsure, it is absolutely within your rights to ask. However, in emergency or urgent situations, your focus should remain on your health, and protections like the No Surprises Act are designed to cover you afterward.
Additional Resources
-
The Centers for Medicare & Medicaid Services (CMS) – No Surprises Act: The official government site with consumer guides and details on your rights. https://www.cms.gov/nosurprises
-
Your State Department of Insurance: Find your state’s regulator to file a complaint or get local guidance. A simple web search for “[Your State] Department of Insurance” will find it.
-
The American Society of Anesthesiologists (ASA) Patient Resources: While geared toward clinical information, it provides valuable context on the profession and standards of care. https://www.asahq.org/madeforthismoment






