Navigating the financial aspect of any medical procedure can feel daunting, and a tonsillectomy is no exception. If you or your child has been recommended for tonsil removal, one of your first questions is likely, “How much will this cost with my insurance?” The answer isn’t a single figure, but a variable one influenced by a tapestry of factors. This guide will demystify the process, providing you with the knowledge and tools to understand your potential financial responsibility, communicate effectively with providers, and plan for this common procedure with confidence.
Cost of Tonsil Removal with Insurance
What is a Tonsillectomy and Why Is It Performed?
A tonsillectomy is the surgical removal of the palatine tonsils, two oval-shaped pads of tissue at the back of the throat. While once an extremely common childhood rite of passage, it’s now performed with more specific medical criteria in mind.
Common reasons for a tonsillectomy include:
-
Recurrent Tonsillitis: Frequent, documented throat infections (e.g., 7+ times in one year, 5+ times per year for two years, or 3+ times per year for three years).
-
Sleep-Disordered Breathing: Enlarged tonsils that obstruct airways, leading to conditions like obstructive sleep apnea, snoring, or troubled breathing during sleep.
-
Chronic Tonsillitis: A persistent infection that doesn’t fully resolve with antibiotic treatment.
-
Abscess or Other Complications: Such as peritonsillar abscess (quinsy) that doesn’t respond to drainage or antibiotics.
-
Suspected Tumor: Though rare, tonsillectomy may be performed for biopsy in cases of suspected malignancy.
Understanding the medical necessity of the procedure, as defined by your insurance plan, is the first critical step in determining coverage.
Key Factors That Influence Your Final Cost
The total expense of a tonsillectomy isn’t just the surgeon’s fee. It’s a sum of several components, each fluctuating based on location, facility, and complexity.
1. The Surgical Setting: Where the Procedure Takes Place
This is one of the largest variables in cost.
-
Hospital Outpatient Department: Often the most expensive setting due to high facility fees.
-
Ambulatory Surgery Center (ASC): Typically more cost-effective than a hospital for routine procedures. Designed for same-day surgeries, their overhead is lower.
-
Surgeon’s Office-Based Facility: The least common for tonsillectronies, but potentially the most affordable if available and appropriate for the patient’s health profile.
2. Provider Fees: Who is Involved in Your Care
You will receive separate bills from different entities:
-
Surgeon’s Fee: For performing the operation.
-
Anesthesiologist’s Fee: For administering sedation or general anesthesia and monitoring you during surgery. Crucially, the anesthesiologist may be out-of-network even if the facility and surgeon are in-network.
-
Facility Fee: Covers the use of the operating room, nursing staff, and standard supplies.
3. Geographical Location
Healthcare costs vary dramatically by state and even by city. Procedures in metropolitan areas or regions with a higher cost of living generally cost more than in rural areas.
4. Surgical Technique and Technology
The method used can impact cost. Traditional “cold” dissection (using a scalpel) may have a different fee structure than methods using coblation (radiofrequency energy) or electrocautery. Newer technologies might carry higher costs but could offer benefits like reduced bleeding or faster recovery.
5. Patient Age and Health Complexity
An adult tonsillectomy is often more complicated and involves a longer, more painful recovery than one for a child, which can affect costs. Pre-existing health conditions may also require additional pre-operative testing or monitoring.
How Health Insurance Works for a Tonsillectomy
Health insurance doesn’t cover 100% of costs (unless you’ve met your out-of-pocket maximum). You pay a portion through a system of deductibles, copays, and coinsurance. Here’s a breakdown of the key terms you must understand:
-
Deductible: The amount you pay for covered services each year before your insurance starts to pay. If your deductible is $1,500, you are responsible for the first $1,500 of eligible medical expenses.
-
Copayment (Copay): A fixed amount you pay for a covered service (e.g., $30 for a specialist visit). For surgery, you may have a copay for the facility.
-
Coinsurance: Your share of the costs after you’ve met your deductible. It’s a percentage. If your coinsurance is 20%, you pay 20% of the allowed amount for the service, and insurance pays 80%.
-
Out-of-Pocket Maximum: The most you’ll have to pay for covered services in a plan year. After you spend this amount, insurance pays 100%.
The Most Important Concept: In-Network vs. Out-of-Network
-
In-Network Providers: Doctors and facilities that have a contracted rate with your insurance company. You pay the least when using in-network providers.
-
Out-of-Network Providers: Those without a contract. Your insurance may pay a smaller percentage or nothing at all, leaving you with significantly higher bills. This is especially risky for anesthesiology services.
Estimating Your Out-of-Pocket Cost: A Step-by-Step Guide
You cannot rely on a simple “average cost.” You must create a personalized estimate.
Step 1: Review Your Insurance Plan Documents.
Locate your Summary of Benefits and Coverage (SBC). Note your:
-
Individual vs. family deductible status (how much you’ve already paid this year).
-
Deductible amount.
-
Coinsurance percentage for outpatient surgery.
-
Copay for outpatient facility.
-
Out-of-pocket maximum.
Step 2: Verify Network Status.
Confirm with your insurance company that:
-
The recommended surgeon is in-network.
-
The surgical facility (hospital or ASC) is in-network.
-
The anesthesiology group that works at that facility is in-network. Call the facility and ask, “Which anesthesia group provides services at your center, and are they in-network for my plan?”
Step 3: Request a Formal Cost Estimate.
-
Ask your surgeon’s office for the CPT code(s) for the planned procedure (e.g., 42820 for tonsillectomy under age 12; 42825 for age 12+; 42826 for tonsillectomy with adenoidectomy).
-
Call your insurance company. Provide the CPT codes, the provider names (surgeon, facility), and ask for a “benefits quote” or “pre-determination.”
-
Ask for the “allowed amount” for each service (surgeon, facility, anesthesia). This is the contracted rate.
-
Ask your surgeon’s office and the facility for a “good faith estimate” (GFE). As of 2022, under the No Surprises Act, healthcare providers are required to give uninsured or self-pay patients a GFE. While not always required for insured patients, many will provide one upon request.
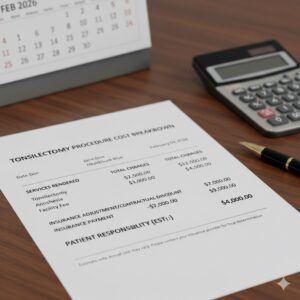
Step 4: Do the Math.
Here is a simplified example for an in-network procedure:
| Cost Component | Allowed Amount (Contract Rate) | Your Responsibility (Assuming $1,500 Deductible Met, 20% Coinsurance) |
|---|---|---|
| Surgeon’s Fee | $900 | You pay 20% = $180 |
| Facility Fee (ASC) | $2,500 | You pay 20% = $500 |
| Anesthesia Fee | $600 | You pay 20% = $120 |
| Pathology Fee (if tonsils are sent to lab) | $150 | You pay 20% = $30 |
| TOTAL ESTIMATED PATIENT RESPONSIBILITY | $830 |
Note: If you have not met your deductible, you would be responsible for 100% of the allowed amounts until the deductible is satisfied.
Comparative Cost Table: Uninsured vs. Insured
The following table illustrates the stark difference between the “sticker price” (chargemaster rate) and the negotiated rate with insurance. These are illustrative national averages.
| Cost Component | Average “Sticker Price” (No Insurance) | Average Allowed Amount (In-Network Insurance) | Patient Savings with In-Network Insurance |
|---|---|---|---|
| Surgeon’s Fee | $1,200 – $2,500 | $800 – $1,200 | ~40-50% |
| Facility Fee (Hospital) | $4,000 – $8,000 | $2,500 – $4,500 | ~35-45% |
| Facility Fee (ASC) | $2,500 – $5,000 | $1,800 – $3,200 | ~30-40% |
| Anesthesia Fee | $800 – $1,500 | $500 – $1,000 | ~35-40% |
| **TOTAL RANGE | $8,500 – $17,000+ | $5,600 – $9,900 | Significant |
Important Note: “An out-of-network provider can create a financial burden that turns a planned procedure into a source of significant stress. Always confirm network status for every professional involved in your care,” advises a patient advocacy specialist.
Strategies to Manage and Reduce Your Tonsillectomy Costs
-
Choose an Ambulatory Surgery Center (ASC): If you are a candidate for an outpatient procedure, an ASC is almost always more affordable than a hospital outpatient department.
-
Ask About Cash-Pay Discounts: If you are uninsured or have a very high deductible, ask the surgeon, facility, and anesthesiologist if they offer a discounted rate for upfront, cash payment. This can sometimes be lower than the insurance-allowed amount.
-
Understand the “No Surprises Act” (2022): This federal law protects you from most surprise medical bills for out-of-network care in emergency situations and for out-of-network providers at in-network facilities without your consent. You must receive advance notice and consent to be treated by an out-of-network provider in non-emergency situations. Read all forms carefully.
-
Payment Plans: Most healthcare providers offer interest-free payment plans. Don’t hesitate to ask about setting up a manageable monthly payment.
-
Health Savings Account (HSA) or Flexible Spending Account (FSA): Use pre-tax dollars from these accounts to pay for your deductible, copays, coinsurance, and even post-op medications and supplies.
The Financial Path: From Pre-Op to Final Bill
-
Pre-Operative Consultation: You may have a copay for this specialist visit.
-
Pre-Op Tests: Any required blood work or EKG will be billed separately.
-
Day of Surgery: You are responsible for your calculated deductible/coinsurance/copay amounts.
-
Post-Op Care: A follow-up visit with the surgeon typically involves a copay. Prescriptions for pain medication and antibiotics are an additional cost.
-
The Bills Arrive: Expect multiple bills over several weeks from the surgeon, the facility, the anesthesiologist, and possibly a pathologist. Review each one carefully for errors. Compare them to your good faith estimate.
-
Explanation of Benefits (EOB): Before you pay, you will receive an EOB from your insurance company for each claim. This is not a bill but a statement showing what was billed, the allowed amount, what insurance paid, and what you owe. Match the “you owe” amount on the EOB to the bill from the provider before paying.
Frequently Asked Questions (FAQ)
Q: What is the average out-of-pocket cost for a tonsillectomy with insurance?
A: There is no true “average” as it depends entirely on your plan. However, for a patient using in-network providers after meeting their deductible, typical out-of-pocket costs can range from $500 to $2,500. If the deductible has not been met, you could be responsible for the entire allowed amount, which could be $4,000-$8,000.
Q: Will my insurance cover a tonsillectomy for sleep apnea?
A: Generally, yes. Sleep-disordered breathing or obstructive sleep apnea documented by a sleep study is a widely accepted reason for medical necessity. Prior authorization from your insurance is almost always required.
Q: How can I avoid a surprise anesthesia bill?
A: This is critical. Once you know your surgical facility, call your insurance company and ask, “Which anesthesia groups are in-network at [Facility Name]?” Then, call the surgeon’s office or facility to confirm which group will be used and verify their network status directly.
Q: Is a tonsillectomy more expensive for adults?
A: Often, yes. The CPT code for patients aged 12 and over has a higher allowed amount due to increased complexity and risk. Recovery can also be longer, potentially leading to more follow-up care.
Q: What if I can’t afford my estimated share of the cost?
A: Talk to the provider’s billing department before the surgery. Be proactive. Explain your situation. They may offer a deeper cash-pay discount, a longer payment plan, or have information on charitable care programs.
Conclusion
Understanding the cost of tonsil removal with insurance requires proactive research and a clear grasp of your own health plan. By verifying network status for all providers, obtaining good faith estimates, and leveraging protective laws like the No Surprises Act, you can transform a complex financial process into a manageable one. The key is to focus not on the total bill, but on your personalized out-of-pocket responsibility, allowing you to make informed decisions and prioritize a smooth recovery.
Additional Resource:
For an official guide to your rights under the No Surprises Act, visit the Centers for Medicare & Medicaid Services consumer website: Consumer Protections Against Surprise Medical Bills






