Dealing with gynecomastia—the enlargement of breast tissue in men—is often more than just a physical concern. For many, it impacts self-esteem, social confidence, and even physical comfort. If you have been researching ways to address this condition, the question of gyno surgery cost with insurance has likely crossed your mind.
While many people assume that “male breast reduction” is strictly a cosmetic procedure, there are several scenarios where health insurance providers may cover part or all of the expenses. This guide provides a deep dive into the costs, insurance criteria, and the steps you can take to make the procedure more affordable.
Gyno Surgery Cost with Insurance
What is the Average Cost of Gyno Surgery?
Before diving into the specifics of insurance, it is helpful to understand the baseline costs. According to recent data from the American Society of Plastic Surgeons and various health cost trackers for 2025-2026, the national average for the surgeon’s fee alone is approximately $4,500 to $6,000.
However, the “sticker price” you see on a surgeon’s website rarely includes everything. The total out-of-pocket cost for a patient paying entirely on their own typically ranges between $6,000 and $12,000.
Breakdown of Typical Surgical Fees
| Expense Component | Estimated Cost Range |
| Surgeon’s Fee | $3,500 – $7,000 |
| Anesthesia Fees | $800 – $1,500 |
| Hospital or Surgical Facility Costs | $1,500 – $3,000 |
| Medical Tests & Lab Work | $200 – $500 |
| Post-Surgery Garments & Meds | $150 – $300 |
| Total Estimated Cost | $6,150 – $12,300 |
Does Insurance Cover Gyno Surgery?
The short answer is: It depends on “Medical Necessity.”
Most insurance companies categorize gynecomastia surgery as a cosmetic procedure if the goal is simply to improve the appearance of the chest. However, they may reclassify it as “reconstructive” or “medically necessary” if the condition causes significant physical symptoms or is tied to an underlying medical issue.
Common Criteria for Insurance Approval
To get the gyno surgery cost with insurance covered, providers like Aetna, Blue Cross Blue Shield, or UnitedHealthcare typically require proof of the following:
-
Persistent Pain: Documentation of chronic pain, tenderness, or discomfort that has not responded to other treatments.
-
Tissue Type: Insurance usually only covers the removal of glandular tissue (true gynecomastia). If the enlargement is purely fat (pseudogynecomastia) caused by weight gain, it is almost always excluded.
-
Duration: The condition must typically be present for at least two years.
-
Rule Out Other Causes: You must prove that the growth isn’t caused by medications, drug use, or hormonal imbalances that could be treated non-surgically.
-
Age and BMI: Some plans require the patient to be over 18 and have a Body Mass Index (BMI) within a certain range to ensure the issue isn’t simply related to obesity.
“The bridge between a ‘cosmetic’ label and a ‘medically necessary’ one is built with documentation. If you can prove that your condition impairs your daily physical function or causes genuine physical pain, your chances of coverage increase significantly.” — Medical Billing Consultant Perspective
Steps to Get Gyno Surgery Covered by Insurance
Navigating the insurance maze requires patience and a proactive approach. Follow these steps to maximize your chances of getting your claim approved.
1. Document Your Symptoms
Start a “health diary.” Note down when you feel pain, skin irritation (intertrigo) under the breast tissue, or if the weight of the tissue causes posture issues. Visit your primary care physician to get these symptoms into your official medical record.
2. Get a Professional Diagnosis
See an endocrinologist or your primary doctor to rule out underlying causes like thyroid issues or pituitary tumors. Insurance companies want to see that you’ve tried to fix the problem without surgery first.
3. Choose a Surgeon Familiar with Insurance
Not all plastic surgeons accept insurance. When booking a consultation, specifically ask: “Do you work with insurance providers for medically necessary gynecomastia cases?” A surgeon who understands the “medical necessity” criteria will know how to take the right photos and write the necessary letters of support.
4. Request a Pre-Authorization
Never assume you are covered until you have a written pre-authorization from your insurer. Your surgeon’s office will submit your records, photos, and a surgical plan to the insurance company for review.
Comparing Gyno Surgery Costs: Insurance vs. Self-Pay
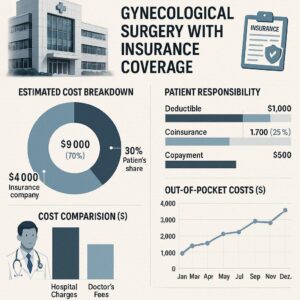
If your insurance does cover the procedure, you won’t necessarily pay zero. You will still be responsible for your deductible and co-insurance.
Cost Comparison Table
| Feature | Insurance Covered | Self-Pay (Out-of-Pocket) |
| Total Bill | $8,000 – $15,000 (Billed to Insurance) | $6,000 – $10,000 (Cash Discount) |
| Your Responsibility | Deductible + Co-pay (e.g., $1,500 – $3,000) | Full Amount ($6,000+) |
| Surgeon Choice | Limited to in-network providers | Any surgeon you choose |
| Wait Time | Longer (due to approval process) | Shorter (schedule at your convenience) |
Important Note for Readers
NOTE: Even if insurance covers the “mastectomy” (tissue removal) part of the surgery, they often consider “liposuction” to be cosmetic. This means you might receive a bill for the liposuction portion of the procedure while the rest is covered. Always ask for a detailed breakdown of what is being submitted to your provider.
Financing Options if Insurance Says “No”
If your claim is denied, do not lose hope. Many patients use alternative methods to manage the cost of gyno surgery.
-
HSA/FSA Accounts: Since gynecomastia is a recognized medical condition (ICD-10 code N62), you can often use pre-tax dollars from a Health Savings Account or Flexible Spending Account.
-
Medical Lending: Companies like CareCredit or PatientFi offer monthly payment plans, sometimes with 0% interest for the first 12–24 months.
-
In-House Financing: Some surgical centers offer their own payment plans to make the procedure more accessible.
FAQ: Gyno Surgery Cost with Insurance
Q: What is the ICD-10 code for gynecomastia?
A: The medical coding for gynecomastia is N62. Having this code on your medical records is the first step toward insurance reimbursement.
Q: Will insurance cover surgery for “puffy nipples”?
A: Usually, no. If the concern is purely aesthetic (puffy nipples or minor contouring), insurance companies almost always classify this as cosmetic.
Q: Can I appeal a denial?
A: Yes. If your insurance denies coverage, you have the right to an appeal. You may need to provide additional evidence, such as ultrasound results showing significant glandular tissue or a letter from a therapist documenting psychological distress.
Q: How much does the consultation cost?
A: Consultations typically cost between $100 and $300. Some surgeons apply this fee toward the total cost of your surgery if you choose to move forward with them.
Conclusion
Navigating the gyno surgery cost with insurance requires a mix of medical evidence and persistence. While many plans default to denying “cosmetic” claims, proving medical necessity through documented pain and glandular growth can save you thousands of dollars. Always start with a thorough medical evaluation and a clear understanding of your specific policy benefits.
Summary: This article explores the average costs of gynecomastia surgery, the specific criteria insurance companies use to determine “medical necessity,” and provides a step-by-step guide for patients to seek coverage. It highlights the difference between glandular and fatty tissue while offering alternative financing solutions for those whose claims are denied.
Additional Resource: American Society of Plastic Surgeons – Gynecomastia Guide






