For healthcare providers, joining insurance networks is a fundamental step in building a practice. Yet, the process of credentialing—the verification of your professional qualifications—is often shrouded in mystery, especially when it comes to cost. It’s rarely a single, straightforward fee. Understanding the true, total cost of credentialing with insurance companies is crucial for accurate financial planning and operational success.
This guide will break down every component of this investment, from hard costs to hidden expenses, providing you with a realistic and comprehensive financial picture.
Cost of Credentialing with Insurance Companies
TABLE OF CONTENTS
ToggleUnderstanding the Credentialing Investment: It’s More Than a Fee
Many practitioners mistakenly believe credentialing costs are limited to a few application fees. In reality, it’s a multi-faceted investment involving direct payments, internal resources, technology, and a significant allocation of time. The total cost is the sum of all these elements, which we will explore in detail.
As one medical practice administrator notes:
“Budgeting for credentialing is like budgeting for a move. You know there will be truck rental, but you forget about the boxes, the time off work, the pizza for helpers, and the two weeks of disorganization. The true cost is in the totality of the process.”
Why a Clear Cost Understanding Matters
Knowing the full expense allows you to:
-
Create an accurate startup or expansion budget.
-
Weigh the return on investment (ROI) for adding each new insurance panel.
-
Decide between handling credentialing in-house versus outsourcing.
-
Avoid cash flow surprises during a critical practice-building phase.
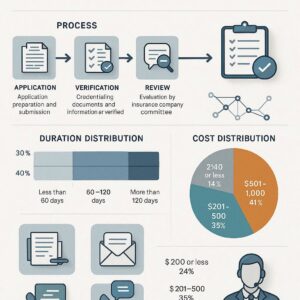
Breakdown of Direct Credentialing Costs & Fees
These are the out-of-pocket, tangible expenses paid to external entities.
1. Primary Source Verification Fees
This is the core of credentialing. Organizations like the National Committee for Quality Assurance (NCQA)-certified Credentials Verification Organizations (CVOs) charge to verify your:
-
Medical education and diplomas
-
Residency training
-
State licenses
-
Board certification status
-
Work history
-
Malpractice insurance history
These fees can range significantly based on the depth of verification required.
2. Council for Affordable Quality Healthcare (CAQH) Profile
While the CAQH ProView system itself is free for providers, there are potential costs:
-
Recredentialing Fees: Some states or plans may charge a small fee for the re-attestation process.
-
Professional Assistance: If you hire a service to set up and maintain your CAQH profile, this becomes an indirect cost.
3. Individual Insurance Company Application Fees
Not all insurers charge an application fee, but many do. These are non-refundable fees paid when you submit your initial credentialing application to participate in their network.
| Payor Type | Typical Fee Range | Notes |
|---|---|---|
| Major National Payors (e.g., Aetna, UnitedHealthcare, Cigna) | $0 – $400 per application | Some have moved away from fees; always check current policy. |
| Blue Cross Blue Shield Plans | $100 – $300 per application | Each state’s independent BCBS plan sets its own fee. |
| Medicaid State Plans | $0 – $250 | Varies dramatically by state; often lower or no fee. |
| Medicare | $0 | CMS does not charge an application fee for individual providers. |
| Smaller/Regional Commercial Plans | $50 – $200 | Common for local HMOs or provider-sponsored plans. |
Important Note: These fees are per provider, per application. Adding a new provider to multiple plans multiplies this cost.
4. State Medicaid Enrollment Fees
For Medicaid, the “credentialing” is often part of the statewide provider enrollment process. Some states mandate an application fee (as permitted by CMS), which is typically standardized.
5. Credentialing Software or Service Subscriptions
In-house credentialing teams often use specialized software to track applications, deadlines, and documents. These platforms charge monthly or annual subscription fees per user or per provider.
The Hidden Costs: Internal Labor & Resource Allocation
This is often the most substantial and overlooked portion of the credentialing cost.
1. Staff Time Expenditure
The credentialing process is notoriously time-consuming. Calculate this cost by multiplying the hours spent by the staff member’s hourly wage + benefits.
-
Initial Application: 2-5 hours per insurance plan (data entry, form completion, compiling documents).
-
Follow-Up & Status Checks: 1-3 hours per plan (phone calls, emails, portal checks).
-
CAQH Maintenance: 1-2 hours quarterly for updates and re-attestation.
-
Recredentialing: 1-3 hours every 2-3 years per plan.
Example Calculation: If your office manager ($25/hour + benefits = ~$35/hr effective) spends 6 hours total on one application, the internal labor cost is $210 for that single plan.
2. Provider Time Cost
Your own time is the most valuable asset. Hours spent filling out detailed histories, locating old documents, and signing forms have a direct opportunity cost—time not spent seeing patients, managing the practice, or with family.
3. Overhead & Operational Drag
Credentialing pulls focus from other revenue-generating or patient-focused activities. It creates administrative drag, slowing down other operations and consuming managerial attention.
Credentialing Service vs. In-House: A Cost Comparison
The decision to outsource is primarily a financial and operational one.
| Cost Factor | In-House Credentialing | Outsourced Credentialing Service |
|---|---|---|
| Direct Fees | You pay all verification and application fees directly. | You still pay all direct fees; the service does not cover these. |
| Labor Cost | High (Staff/Provider time). Variable, hidden in payroll. | Replaced by a fixed, known service fee. |
| Service Fee | None (but software subscription possible). | Typically $200 – $800 per provider, per plan. Often tiered packages. |
| Speed & Efficiency | Dependent on staff bandwidth and expertise. Can be slow. | Usually faster due to specialization and dedicated resources. |
| Expertise | Must be developed internally. Risk of errors. | High. Specialists know payer-specific requirements and nuances. |
| Follow-Up Burden | Entirely on your staff. | Handled by the service, a major time savings. |
Key Takeaway: Outsourcing converts a high, variable, hidden labor cost into a known, fixed expense. It is often cost-effective for practices adding multiple providers or plans simultaneously, or for those without dedicated administrative bandwidth.
The “Opportunity Cost” of Delayed Revenue
This is the most critical financial concept in credentialing. Opportunity cost refers to the revenue you lose while waiting to be credentialed and able to bill.
-
Scenario: A new psychiatrist is ready to see patients but spends 90 days in the credentialing process with a major insurer. They could realistically see 20 patients per week at an average net reimbursement of $150 per visit.
-
Lost Revenue Calculation: 20 patients/week x $150 x 12 weeks = $36,000 in unrealized revenue.
-
This dwarfs almost any direct credentialing cost. Expediting the process, whether through meticulous in-house management or a skilled service, directly mitigates this massive opportunity cost.
Cost-Saving Strategies for Efficient Credentialing
-
Prioritize Key Payers: Don’t apply to every plan at once. Research which 3-4 plans cover the majority of your target patient population and start there.
-
Impeccable Documentation: Create a “master credentialing packet” with notarized copies of every document (license, DEA, diploma, malpractice, etc.). Perfect applications avoid delays.
-
Leverage CAQH Fully: Keep your CAQH profile 100% updated at all times. This is the source for most payers, and inaccuracies cause immediate setbacks.
-
Systematic Tracking: Use a simple spreadsheet or dedicated software to track application dates, contacts, and follow-up deadlines for every plan.
-
Batch Applications: If adding a new provider, submit applications to all targeted payers simultaneously to start the parallel processing clocks.
-
Negotiate with Service Providers: If outsourcing, ask if they offer volume discounts for multiple providers or a bundled package for initial credentialing + CAQH maintenance.
Calculating Your Return on Investment (ROI)
Credentialing is an investment, and its ROI should be evaluated.
-
Cost Side (Sum of): Direct Fees + Internal Labor Cost (or Service Fee) + Software Costs.
-
Revenue Side: Estimate the monthly revenue you expect from being in-network with that payer (e.g., # of expected patients x avg. reimbursement).
-
ROI Time: Divide your Total Cost by your Expected Monthly Revenue from that payer. This gives you the number of months to “break even” on the credentialing investment.
Example: If credentialing with Payer X costs $1,000 total and you expect $2,000/month in revenue from them, your credentialing investment is recouped in two weeks of seeing their patients. This makes the cost negligible in the long run.
Conclusion
The true cost of credentialing with insurance companies is a composite of direct fees, substantial internal labor, and the critical opportunity cost of delayed revenue. By understanding this full financial picture, healthcare providers can make informed decisions, budget effectively, and implement strategies to streamline the process. Viewing credentialing not as a mere expense but as a necessary and calculable investment in your practice’s financial pipeline is the key to managing it successfully.
Frequently Asked Questions (FAQ)
Q: What is the single most expensive part of credentialing?
A: For most practices, it’s the opportunity cost of delayed revenue while waiting for approval. The internal staff time required to manage the process is the second largest, often overlooked, expense.
Q: Are credentialing costs tax-deductible for healthcare providers?
A: Yes, typically. Costs associated with professional licensing, credentialing, and joining insurance networks are generally considered ordinary and necessary business expenses and are tax-deductible. Always consult with your CPA.
Q: How can I reduce the time cost of credentialing?
A: Preparation is key. Maintain a perfectly updated CAQH profile and a ready digital packet of all required documents. Proactive, calendar-driven follow-up (calling weekly) can also shave weeks off the process. Consider outsourcing for the most time-efficient solution.
Q: Does it cost money to recredential?
A: Usually, there are no large direct fees for recredentialing (every 2-3 years). However, the internal labor cost to complete the process and the cost of any CAQH maintenance services reapplies.
Additional Resources
-
Council for Affordable Quality Healthcare (CAQH) ProView: The official portal for creating and maintaining your central credentialing profile. https://proview.caqh.org
-
Centers for Medicare & Medicaid Services (CMS) Provider Enrollment: Essential information and forms for Medicare and Medicaid enrollment. https://www.cms.gov/medicare/provider-enrollment-and-certification






