If you or your child needs a tonsillectomy, the medical necessity is clear, but the financial picture often feels cloudy. “How much will I actually pay?” is the pressing question. While insurance is a crucial safety net, it doesn’t mean the procedure is free. This guide will demystify the tonsil removal cost with insurance, helping you understand your potential financial responsibility and navigate the process with confidence.
Understanding these costs upfront can prevent stressful surprises and allow you to plan effectively. We’ll break down the variables, from deductibles to surgeon fees, and provide you with a practical framework for getting to your bottom line.
Cost of Tonsil Removal with Insurance
TABLE OF CONTENTS
ToggleHow Health Insurance Works with Surgery: Key Concepts
Before diving into specific numbers, you must grasp the basic mechanics of your health insurance plan. These components directly determine your out-of-pocket costs.
Deductible, Copay, and Coinsurance: The Cost-Sharing Trio
Your share of the cost is typically defined by three main terms:
-
Deductible: The amount you pay for covered services each year before your insurance starts to pay. If your deductible is $1,500, you pay 100% of allowed charges until you’ve spent that amount.
-
Copay (Copayment): A fixed amount you pay for a covered service, like a doctor’s visit. For surgery, you might have a copay for the initial consultation.
-
Coinsurance: Your share of the costs after you’ve met your deductible, shown as a percentage. If your coinsurance is 20%, you pay 20% of the allowed amount for the service, and your insurance pays 80%.
In-Network vs. Out-of-Network: A Critical Distinction
This is perhaps the most significant factor affecting your tonsil removal cost with insurance.
-
In-Network: Providers (surgeons, anesthesiologists, facilities) have negotiated discounted rates with your insurance company. You pay the lowest out-of-pocket costs.
-
Out-of-Network: Providers have not agreed to these rates. Your insurance may pay much less or nothing at all, leaving you responsible for a much larger bill, often at the provider’s full “sticker price.”
Out-of-Pocket Maximum: Your Financial Safety Net
This is the absolute limit you will pay in a policy year for covered services. Once you hit this amount through deductibles, copays, and coinsurance, your insurance pays 100% of allowed charges. Knowing this figure is key to understanding your worst-case financial scenario.
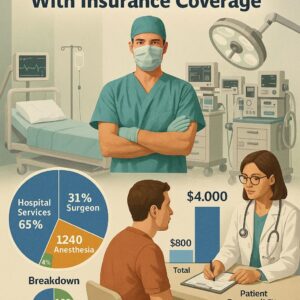
Breaking Down the Components of a Tonsillectomy Bill
A tonsillectomy isn’t a single charge. It’s a bundle of services, each billed separately. Understanding these components helps you see where the money goes.
1. Surgeon’s Fee
This covers the otolaryngologist’s (ENT surgeon) expertise and performance of the procedure. The fee varies based on the surgeon’s experience, geographic location, and the complexity of the case.
2. Anesthesia Fee
An anesthesiologist or nurse anesthetist administers sedation and monitors you during surgery. This is a separate fee, and it’s crucial to ensure this professional is also in-network.
3. Facility Fee
This is the cost of using the hospital or ambulatory surgical center (ASC). It covers the operating room, nursing staff, equipment, and recovery room. Facility fees at an ASC are generally significantly lower than at a hospital.
4. Pre-Operative and Post-Operative Costs
These include:
-
The initial consultation and diagnostic tests.
-
Any prescribed medications for recovery (pain relievers, antibiotics).
-
Follow-up appointment(s).
Estimated Cost Ranges with Insurance: A Realistic Look
Providing a single number is impossible due to plan variability, but we can illustrate with realistic scenarios. The table below compares two common insurance plan types.
Estimated Out-of-Pocket Cost Scenarios for Tonsillectomy
| Cost Component | Scenario A: High-Deductible Plan (Deductible: $3,000) | Scenario B: Low-Deductible PPO Plan (Deductible: $500) |
|---|---|---|
| Total Allowed Charges (In-Network) | $7,500 | $7,500 |
| Your Deductible Status | Not yet met | Already met |
| Your Payment for Surgery | You pay the first $3,000 (deductible). Then, you may pay coinsurance (e.g., 20% of remaining $4,500 = $900). Total Estimate: $3,900 | You pay only coinsurance (e.g., 20% of $7,500 = $1,500). Total Estimate: $1,500 |
| Key Consideration | You are responsible for 100% of costs until you hit your high deductible. | Your costs are lower per procedure, but these plans often have higher monthly premiums. |
Important Note: “These estimates assume all providers and the facility are in-network. The single biggest financial mistake a patient can make is receiving care from an out-of-network provider during an in-network procedure, a situation known as ‘surprise billing.’ Always verify each professional involved,” advises a healthcare financial advocate.
Factors That Influence Your Final Cost
-
Geographic Location: Costs are higher in urban areas and certain regions of the U.S.
-
Type of Facility: An Ambulatory Surgery Center (ASC) is almost always less expensive than a hospital outpatient department for the same procedure.
-
Medical Complexity: Cases involving severe sleep apnea, excessive bleeding risk, or other complications may incur higher costs.
-
Your Insurance Plan’s Specific Contract: Even within “in-network,” different plans have different negotiated rates.
A Step-by-Step Action Plan to Determine Your Cost
Don’t guess. Follow this proactive plan to get the clearest possible picture.
Step 1: Review Your Insurance Plan Documents
Locate your Summary of Benefits and Coverage (SBC). Identify your:
-
Individual deductible amount and how much you’ve met this year.
-
Coinsurance percentage for surgical procedures.
-
In-network vs. out-of-network cost-sharing.
-
Out-of-pocket maximum.
Step 2: Obtain the Procedure Codes from Your Surgeon’s Office
The coder at your ENT’s office can provide you with the anticipated CPT (Current Procedural Terminology) codes. The primary code is usually 42826 (Tonsillectomy, primary or secondary; age 12 or over) or 42825 (for under age 12). There may also be codes for adenoid removal.
Step 3: Contact Your Insurance Company
Call the member services number on your insurance card. Provide them with:
-
The CPT codes.
-
The name and Tax ID of your surgeon and preferred facility (hospital or ASC).
-
Ask for a “pre-service cost estimate” or “benefits verification.”
Questions to Ask: -
“Are the surgeon, anesthesiologist, and facility in-network?”
-
“What is the allowed amount for each of these codes?”
-
“Given my current deductible status, what will my coinsurance responsibility be?”
-
“Is prior authorization required for this procedure?”
Step 4: Contact the Hospital or ASC Billing Department
Ask for an estimate based on the codes and your insurance information. Inquire about:
-
Payment plan options if you will have a large balance.
-
Any potential for a prompt-pay discount if paying upfront in full.
Strategies to Manage and Reduce Your Out-of-Pocket Costs
If the estimated cost is daunting, consider these approaches:
-
Schedule Strategically: If you’ve already met your deductible for the year, scheduling the procedure before the plan year resets can save you thousands.
-
Choose an Ambulatory Surgery Center (ASC): Politely ask your surgeon if the procedure can be safely performed at an in-network ASC instead of a hospital.
-
Negotiate a Payment Plan: Most provider billing departments offer interest-free payment plans. Set this up before the procedure to avoid collections.
-
Ask About Cash-Pay Discounts: In rare cases, if your deductible is extremely high, the cash price (without insurance) might be lower than the insurance-adjusted price. This is complex and requires careful comparison.
-
Utilize a Health Savings Account (HSA) or Flexible Spending Account (FSA): Use these pre-tax dollars to pay for eligible expenses, effectively giving you a discount equal to your tax rate.
Conclusion
Understanding the cost of tonsil removal with insurance requires moving beyond your policy’s basics to engage proactively with both your insurer and providers. By mastering your plan’s details, obtaining procedure codes, and securing formal estimates, you can transform an ambiguous potential expense into a manageable, planned cost. This knowledge empowers you to make informed decisions, explore cost-saving options like ASCs, and focus on what truly matters—a successful recovery.
Frequently Asked Questions (FAQ)
Q: What is the average copay for a tonsillectomy?
A: Pure copays for surgeries are less common. You’re more likely to have a coinsurance responsibility (like 20%) after meeting your deductible. You may have a copay for the pre-op and post-op office visits.
Q: Can I get a tonsillectomy covered if it’s for recurrent strep throat and not sleep apnea?
A: Yes. Most insurers follow clinical guidelines that cover tonsillectomy for recurrent throat infections (e.g., 7+ episodes in one year, 5+ per year for two years, etc.). Prior authorization from your doctor is typically required.
Q: What happens if I get a bill from an out-of-network anesthesiologist?
A: This is a “surprise bill.” New federal and state laws offer protections against this. Contact your insurer first to dispute it, then the provider. You may only be responsible for in-network cost-sharing amounts.
Q: How long does it take to get bills after a tonsillectomy?
A: Bills trickle in separately over several weeks to months. You may receive bills from the surgeon, anesthesiologist, facility, and lab. Don’t be alarmed by the “total charge” on the initial statement; wait for the Explanation of Benefits (EOB) from your insurance, which shows your true responsibility.
Additional Resources
-
Healthcare.gov Glossary: A clear, official guide to health insurance terms and concepts. https://www.healthcare.gov/glossary/
-
Patient Advocate Foundation: A non-profit that provides case management and financial assistance to patients. https://www.patientadvocate.org/